Abstract
Background:Achievement of MRD-negative status in MM patients following auto-HSCT is a prognostic factor that has a positive effect on relapse-free survival (RFS). However, the time after which the loss of MRD-negative status occurs have not been established so far. The duration of MRD-negative status can be expected to allow determination of the necessity and duration of maintenance therapy (MT) received by MM patients who have achieved a stringent complete remission (CR) following auto-HSCT.
Aims: To evaluate the duration of MRD-negative status achieved in MM patients following auto-HSCT; to assess the effects of MRD-negative status achievement on RFS and treatment-free survival (TFS).
Patients and Methods: From March 2014 to October 2016, 29 patients with MM (12 males and 17 females) aged 40 to 66 years (median 56 years) who had achieved CR, following auto-HSCT, were enrolled in this prospective study. Disease stages (ISS) were as follows: stage I, II and III were observed in 9, 11 and 9 patients, respectively. Induction of remission included bortezomib-containing regimens (VCD, PAD) in all 29 patients. Immunomodulatory drugs and bendamustine were each used twice. Distribution of patients by type of anti-tumor responses (IMWG) after induction was as follows: CR, very good partial remission and partial remission were observed in 16 (55%), 12 (41%) and 1 (4%) patients, respectively. Single and tandem auto-HSCT were conducted in 25 and 4 patients, respectively. In order to determine MRD status, bone marrow examination using a six-color flow cytometric assay was performed on Day 100 following auto-HSCT with the use of an antibody panel to the following antigens: CD38, CD138, CD45, CD56, CD117, CD19. MRD-negative status was defined as presence of less than 20 clonal plasmatic cells among 2,000,000 white blood cells (<0.001%, detection limit - 10-5).
After auto-HSCT, all patients were followed up and received no MT. The analysis of MRD status was conducted every 3 months until the development of a disease relapse with the use of a six-color flow cytometric assay. The follow-up period since the moment of MRD detection on Day 100 following auto-HSCT was 3 to 33 months (median value = 12 months). The evaluated parameters included the time to loss of MRD-negative status (period since the moment of detection of MRD-negative status on Day 100 following auto-HSCT till the appearance of minimal residual population), RFS (period since the moment of detection of MRD-status on Day 100 following auto-HSCT till the assertion of a disease relapse according to IMWG 2014 criteria), TFS (period since the moment of detection of MRD-negative status on Day 100 following auto-HSCT till the initiation of the next line of therapy). Statistical analysis was done using SAS 9.4. The compared groups were overall balanced for known significant factors.
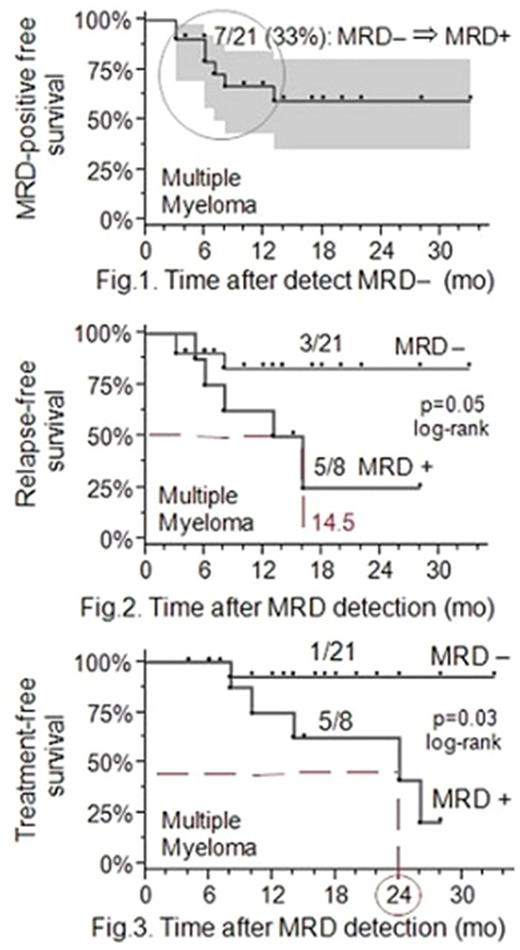
Results: Following auto-HSCT, stringent CR was achieved in 21 (72%) patients, while MRD-positive status was detected in 8 (28%) cases. Loss of MRD-negative status was ascertained in 7 (33%) out of 21 patients during the period from 3 to 13 months. MRD positive free survival was 60% within 33 months (Fig. 1).
Immunochemical disease relapse was established in 3 (15%) patients with MRD-negative status and 5 (63%) patients with MRD-positive status achieved after auto-HSCT. Two-year RFS in patients with MRD-positive status was significantly lower compared to the patients with MRD-negative status: 25% vs. 80% (log-rank test, p=0.05, hazard ratio = 2.5, 95% CI = 0.9-6.4) (Fig. 2).
TFS was significantly higher in patients with MRD-negative status achieved after auto-HSCT: 90% versus 20% within 28 months (p=0.03). It should be noted that only one patient from MRD-negative group required the initiation of the next line of therapy throughout the entire follow-up period as compared to 5 (63%) patients in MRD-positive group (Fig. 3).
Conclusion: The values of time to loss of MRD-negative status in MM patients following auto-HSCT, which were determined in the study, confirmed the hypothesis of favorable prognosis without the use of MT. Prescription of additional treatment to patients who have achieved a stringent complete remission after auto-HSCT does not have any pathogenetical basis, is related to the risk of adverse events and requires the use of concomitant therapy. High values of RFS and TFS rates observed in patients with MRD-negative status following auto-HSCT also confirm our hypothesis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal